Heading off headache
INTRODUCTION
Headache, an almost universal human experience, is one of the most common complaints encountered in
medicine and neurology. The evaluation of this condition may be straight forward or challenging, and, though often benign, the headache may prove to be an ominous symptom.
With a lifetime prevalence of 93 % in men and 99 % in women, headaches are undeniably an extremely common problem. They are often correlated with stress, tension, and a litany of existing medical conditions. Often, patients will live with headache pain for months or even years before seeking care. Over the counter remedies like aspirin, ibuprofen, and acetaminophen are often used to reduce symptoms of pressure and pain prior to seeking medical advice.
Here I'll be discussing two difficult and controversial headache syndromes, tension-type headache and cervicogenic headache.
 |
| Hypothesis for tension-type & cervicogenic headache |
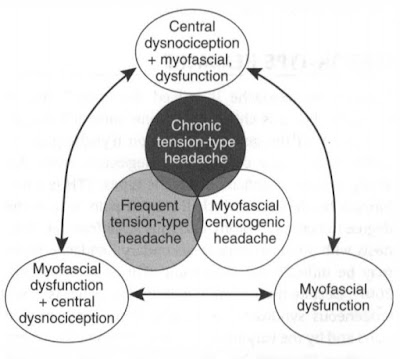
Tension-type headache:
Tension-type headache is indeed the most common headache, but it is chiefly its chronic form (CTTH), affecting 3 % of the general population. A tension headache is generally a diffuse, mild to moderate pain in your head that's often described as feeling like a tight band around your head.
Signs and symptoms of a tension headache include:
- Dull, aching head pain
- The sensation of tightness or pressure across your forehead or on the sides and back of your head
- Tenderness on your scalp, neck, and shoulder muscles.
Cervicogenic headache:
Cervicogenic headaches that refer pain from structures in the cervical spine region (e.g., joints, muscles, nerves) Cervicogenic headaches can mimic migraines, so it will be more difficult to distinguish a cervicogenic headache from a migraine headache. The primary difference is that a migraine headache is rooted in the brain, and a cervicogenic headache is rooted in the cervical spine (neck) or base of the skull region. Prevalence estimates for cervicogenic headache range from 0.4 % to 4.1 %.
Sign and symptoms of a cervicogenic headache:
- pain on one side of your head or face
- a stiff neck
- pain around the eyes
- pain while coughing or sneezing
- a headache with certain neck postures or movement.
 |
| Pattern of headache |
EPIDEMIOLOGY
The lifelong prevalence of headache is 96%, with a female predominance. The prevalence of tension-type headache is approximately 40% and migraine 10%. Migraine occurs most commonly between the ages of 25 and 55 years and is 3 times more common in females. It can cause significant disability, migraine remains underdiagnosed and underrated. Trigeminal autonomic cephalgias are rare compared with migraine and tension-type headache. The most common trigeminal autonomic cephalgia is cluster headache, with a population prevalence of 0.1% and a male/female ratio of 3.5-7:1.
Chronic daily headache, daily or near-daily headache for months to years, is widely reported in the literature, yet is not an official diagnosis in the International Classification of Headache Disorders. Chronic daily headaches of long duration include chronic migraine, chronic tension-type headache, hemicrania continua, and new daily persistent headache. Worldwide prevalence of chronic daily headache has been consistent at 3%-5%,4 most of which likely represents chronic migraine.
 |
| Algorithm for headache diagnosis |
CLASSIFICATION OF HEADACHE
Primary headache
A primary headache has no known underlying cause.
1. Migraine
2. Tension·type headache
3. Cluster headache and other trigeminal autonomic cephalalgias
4. Other primary headaches
Secondary headaches
It is the result of another condition causing traction on or inflammation of pain-sensitive structures.
1. Headache attributed to head and/or neck trauma
2. Headache attributed to a cranial or cervical vascular disorder
3. Headache attributed to nonvascular intracranial disorder
4. Headache attributed to a substance or its withdrawal
5. Headache attributed to infection
6. Headache attributed to disorder of homeostasis
7. Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth, or other facial or cranial structures
8. Headache attributed to psychiatric disorder Cranial neuralgias, central and primary facial pain,
and other headaches
9. Cranial neuralgias and central causes of facial pain
10. Other headaches, cranial neuralgia, central or primary facial pain
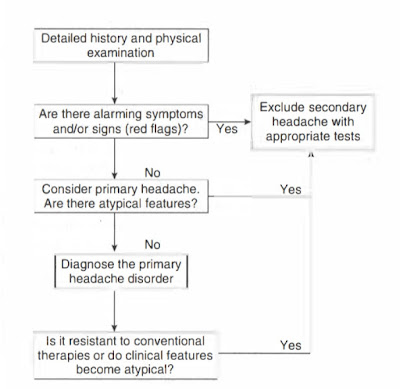
IMPORTANT ELEMENT OF THE HEADACHE HISTORY
• Family history of migraine
• Childhood migraine proxy symptoms: carsickness, gastrointestinal complaints
• Age of onset
• Frequency, severity, and tempo over time
• Triggering, aggravating, or alleviating features
• Autonomic features
• Aura features
• Current and prior treatments
• Lifestyle features
• Comorbid conditions
PHYSICAL EXAMINATION

HEADACHE "RED FLAGS"
• New headache in older patients
• Abnormal neurologic examination including papilledema and change in mental status
• New change in headache pattern or progressive headache
• New headache in the setting of HIV risk factors, cancer, or an immunocompromised status
• Signs of a systemic illness (eg, fever, stiff neck, rash)
• Triggered by cough, exertion, Valsalva maneuver
• Headache in pregnancy/postpartum period
• First or worst headache
PHYSIOTHERAPY MANAGEMENT OF HEADACHE
It is the most commonly used non-pharmacologic treatment of TTH. Cervical exercises, relaxation, massage, postural exercises, craniocervical techniques, thermotherapy, vertebral mobilization, and stretching are effective in reducing TTH symptoms such as pain frequency and intensity. In the studies that have applied joint mobilization, the cervical range of motion has improved.
3 effective ways to treat headache:
1. Manual therapy
Proven hands-on techniques are designed to alleviate joint and muscle stiffness, increase the mobility of the head and neck, decrease muscle tension and spasms, and improve muscle performance.
2. Exercise
Research has shown that various types of specific exercises will decrease pain, improve endurance, decrease inflammation, and promote overall healing. In addition to individualized prescribed exercises, customized home-exercise programs are an essential part of the treatment plan.
3. Education
Educational strategies have been found helpful at lessening the severity and/or frequency of headaches. These strategies include identifying highly individualized triggers (ie, dietary, sleep, movement/postural habits, stressors, hydration). Effective strategies to alleviate symptoms also include a wide variety of relaxation techniques.
Nice bhna 👏
ReplyDelete